Abstract
Background
The standard practice for diagnosis of heparin-induced thrombocytopenia (HIT) involves a combination of 4T score and laboratory tests, such as enzyme immunoassay for detection of antibodies. We noted a lack of widespread use of 4T score in our practice setting. We also found that our laboratory utilized Particle Immunofiltration Assay (PIFA) for HIT screening, which has been shown to have questionable diagnostic utility in HIT diagnosis (Warkentin et al., 2007). The study aims to improve the rate of 4T score usage in conjunction with an improved laboratory diagnostic test for patients with suspected HIT in a cost-efficient manner.
Method
We initiated a quality improvement project involving the review of all patients with laboratory orders for PIFA testing between March 2017 to March 2018, explicitly assessing for documented 4T scores before the ordering of PIFA. Three of the investigators also calculated 4T scores for these patients at the time of laboratory testing and noted the results of the serotonin release assay (SRA), if ordered. We further collected data on any alternative anti-coagulation used in such patients for a cost-efficacy analysis later.
Results
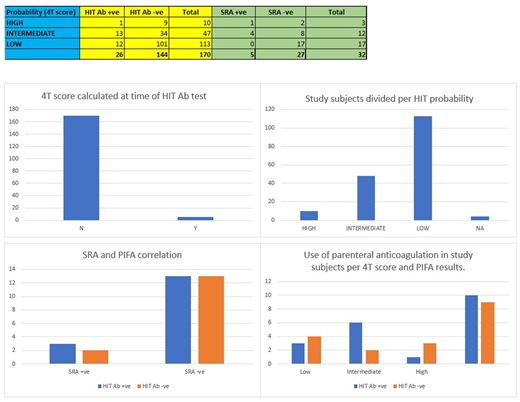
A total of 170 PIFA tests were ordered during the period of investigation. Only five (0.02%) of these patients had a documented 4T score at the time of testing. One hundred thirteen patients (66.4%) had a low 4T score per investigator-calculation. Forty-seven patients (27.6%) were noted to have intermediate 4T scores. Lastly, ten patients (0.05%) were observed to have high 4T scores. A total of 32 SRAs were ordered; five of which were positive (four with an intermediate 4T score and one with high 4T score). PIFA was false-negative in two confirmed cases of positive SRA and false-positive in 13 instances of negative SRA. Thus, in this study, the sensitivity of PIFA was noted to be 60%, and specificity was observed to be 50%. Nineteen patients also received alternative parenteral anti-coagulation (fondaparinux or argatroban); seven of these were with low, eight with intermediate, and four with high 4T scores.
Conclusion
The study highlights the need for improving 4T score usage rates in our hospital as well as a need for switching to an alternative HIT screening test to promote patient safety and cost efficacy. Hence, we have begun the integration of 4T score with laboratory testing into the electronic medical record, alongside a shift in our HIT screening test from PIFA to the recently FDA-approved automated latex immunoturbidimetric assay. We will be continuing analysis of patients with suspected HIT for another six months to assess the effects of the above interventions.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.